Lasers have multiple uses in surgical periodontics. Advantages of laser therapies over conventional periodontal surgery center on six major areas:
Although an association between use of lasers and altered wound healing has been recognized, with use of optimal settings for a given procedure, laser therapy will result in wound healing comparable to or better than (i.e., accelerated) that observed with conventional surgery (Figure 4-1). Studies on wound healing with lasers (Nd:YAG, diodes, CO2) versus the scalpel generally show an initial lag in soft tissue wound healing but equivalence within 2 weeks of postoperative observation. Many of these studies were done more than a decade ago with units that emitted much higher fluences than current lasers. Studies performed with more modern equipment by the more knowledgeable researchers of today might show equivalence between scalpel and laser wound healing within 24 h of the incision.
The specific objectives of planned laser procedures must be considered on a wavelength-by-wavelength basis; results of CO2 laser wound studies cannot be extrapolated to those for Nd:YAG, diodes, or erbium wavelengths. As with all “hi-tech” devices and instruments, the results depend greatly on the expertise of the user, for whom appropriate training is essential to develop the requisite clinical skills and a sound knowledge base that includes optimal settings for watts (W), millijoules (mJ), hertz (Hz), duty cycle, pulse width, hand speed, and other parameters.

Figure 4-1 Periodontal laser treatment for a tight lingual frenum. The patient was referred by a speech pathologist for surgical correction. A, Presurgical view of the frenum. B, Beginning incision for release of lingual frenum with CO2 laser. Note excellent hemostasis and conservative incision. C, Immediate postoperative view of completed lingual frenectomy. D, Lingual frenectomy site 3 days after surgery. Note excellent and rapid healing. © Dr. Robert A. Convissar.
Many laser procedures avoid extensive flap reflection and significant trauma to the wound area. Accordingly, with minimal invasive site preparation, the inflammatory response is decreased, resulting in greater patient comfort. Decreased pain and swelling result from laser sealing of the lymphatics and nerve endings. Biostimulation of the wound area and enhanced wound healing also may occur.
The Nd:YAG and diode lasers emit wavelengths that are absorbed more readily in pigmented tissues, such as tissues with a high concentration of hemoglobin. Use of these lasers, therefore, creates a hemostatic environment during and immediately after surgery as the hemoglobin absorbs the laser energy. CO2 lasers accomplish hemostasis through a different mechanism: When collagen in the walls of the blood vessels absorbs the CO2 wavelength, the helical collagen polymer unravels. With this altered conformation, the collagen fibers shrink, causing the lumens of the blood vessels to shrink, with consequent hemostasis.
Therefore significant hemostasis can be achieved in laser procedures, especially in medically compromised patients (Figure 4-2). Preoperatively, the medical history often reflects extensive pharmaceutical intervention to provide anticoagulation, including prophylactic aspirin and platelet aggregation inhibitors. Patients also may be using many “natural” homeopathic remedies and other preparations that may interfere with clotting. They may not identify the use of these over-the-counter (OTC), nonprescription preparations in the medical or drug history. Such compounds as curry powder, cayenne pepper, cinnamon, and other herbs and spices have a high salicylate content, which can affect clotting. Ginkgo biloba, vitamin E, and other preparations available in health food stores and pharmacies also are associated with impaired clotting.
When scalpel procedures must be avoided in a patient with coagulation considerations, lasers allow surgery to proceed without compromising the patient’s overall health. In the past, the anticoagulant therapy regimen would have been modified and extensively monitored. With lasers, anticoagulant therapy is much less of an issue during treatment.
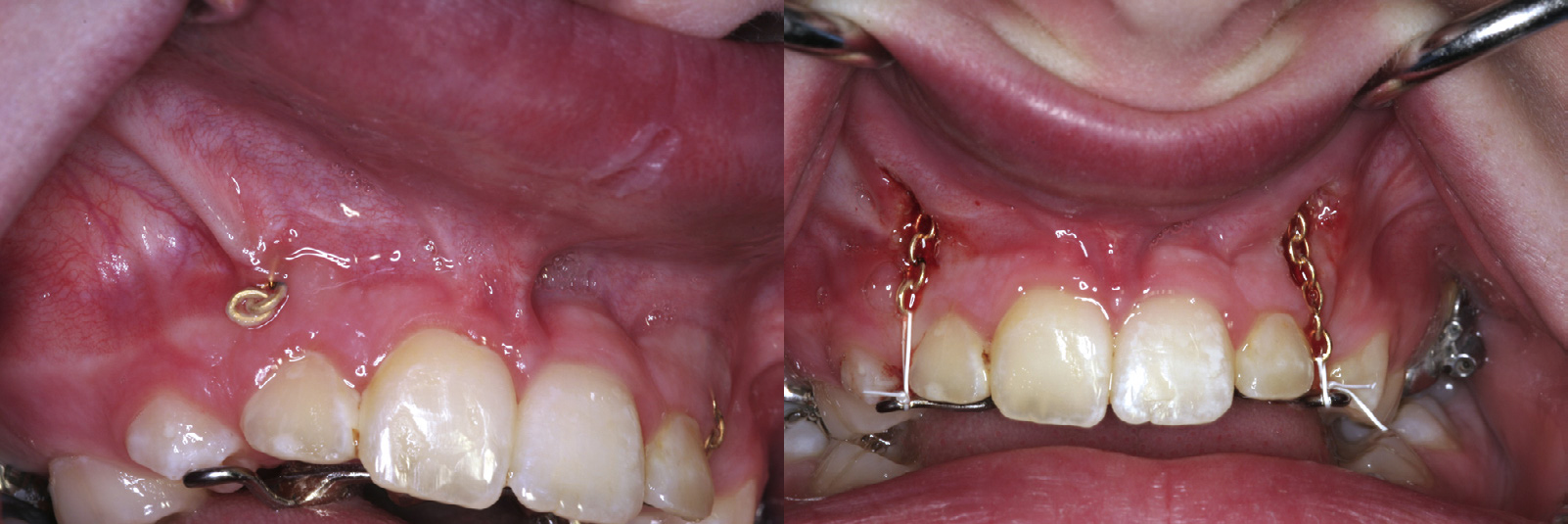
Figure 4-2 Use of a laser to gain adequate intraoral surgical access in a medically compromised patient on anticoagulation therapy. A, Presurgical view of a buried orthodontic chain. B, Immediate postoperative view after exposure of the orthodontic chain accomplished by means of a laser. The laser tip was moved in an apical direction while tension was placed on the exposed chain. With minimal hemorrhage, clear access to the wound area has been obtained. The chain can now be successfully incorporated into the orthodontic appliance.
Some superficial soft tissue procedures can be performed with use of commercially available topical anesthetics, such as those containing lidocaine and prilocaine. Orthodontic and pediatric patients requiring frenectomy and gingivoplasty or gingivectomy are especially suitable candidates for laser procedures with topical anesthesia.
With use of loupes with at least 3× magnification, sulcular laser procedures with small-spot-size laser tips can be performed without gingival flap reflection. This may be applied to procedures such as sulcular debridement and some limited crown-lengthening procedures.
Knowledge of laser physics is a prerequisite to successful clinical application and generally is acquired through laser certification courses. Familiarity with the properties of each wavelength, including depth of penetration of different tissue types, is essential for the practitioner in determining the optimal laser treatment, to maximize the quality of results. In addition, implementation of specific safety protocols, including the designation of a laser safety officer, is mandatory in any clinical setting in which a laser is used. Laser safety education is a requirement for all dental surgery team members.